- Home
- About
- Hospitals
-
Treatments
- Orthopedic & Spine
- Knee Replacement
- Carpal Tunnel Release
- Rotator Cuff Repair
- Meniscus Repair / Meniscectomy
- Total Hip Replacement (THR)
- Total Shoulder Replacement
- Arthroscopy
- Ligament Reconstruction
- Spinal Fusion
- Discectomy
- Laminectomy
- Spinal Decompression
- Vertebroplasty and Kyphoplasty
- Fracture Repair
- ACL Reconstruction
- Tendon Repair
- Osteotomy
- Amputation
- Pediatric and Adult Cardiac
- Neuroscience
- Oncology
- Nephrology & KTP
- Gastroenterology & Hepatobiliary
- Obstetrics and Gynaecology
- Infertility
- Dental & Maxillofacial
- Plastic & Cosmetic Surgery
- Rhinoplasty
- Blepharoplasty (Eyelid Surgery)
- Facelift (Rhytidectomy)
- Breast Augmentation (Mammoplasty)
- Breast Reduction (Mammoplasty)
- Breast Lift (Mastopexy)
- Liposuction
- Abdominoplasty (Tummy Tuck)
- Brazilian Butt Lift (BBL)
- Lip Augmentation
- Breast Reconstruction
- Cleft Lip and Palate Repair
- Scar Revision
- Burn Reconstruction
- Botox Injection
- Ophthalmology
- Otolaryngology (ENT)
- Endocrinology
- General and Minimal Invasive Surgery
- Pulmonology
- Rheumatology
- Urology
- General Medicine
- Multispecialty
- Orthopedic & Spine
- Doctors
- Contact Us
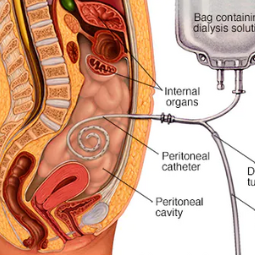
Peritoneal Dialysis
Peritoneal Dialysis (PD) is a medical treatment for patients with kidney failure or
end-stage renal disease (ESRD). It is an alternative to hemodialysis, providing
a way to remove waste products and excess fluids from the bloodstream when the
kidneys are no longer able to perform these essential functions. Peritoneal
dialysis uses the lining of the abdominal cavity (peritoneum) as a natural
filter to perform the cleansing process. Here's an overview of peritoneal
dialysis:
Purpose: The primary purpose of peritoneal dialysis
is to replace the normal filtration function of the kidneys. It helps to remove
waste products, excess salts, and fluids from the bloodstream while maintaining
the balance of electrolytes and controlling blood pressure.
Procedure:
- Catheter Placement: To undergo peritoneal dialysis, a patient first needs to have a soft, flexible catheter surgically implanted into the abdominal cavity. This catheter has two parts: one end protrudes from the abdomen and the other remains within the abdominal cavity.
- Dialysis Solution: Peritoneal dialysis involves the use of a special dialysis solution (dialysate) that contains a specific concentration of electrolytes. The dialysate is introduced into the peritoneal cavity through the catheter and remains there for a specified period.
- Peritoneum Filtration: The peritoneum lining the abdominal cavity acts as a natural filter. Waste products and excess fluids from the bloodstream move across the peritoneum into the dialysate, effectively cleansing the blood.
- Draining the Dialysate: After a set period, the dialysate is drained from the abdominal cavity through the catheter and disposed of. This process is typically repeated several times a day, and the frequency and duration of these exchanges are determined by a nephrologist based on the patient's kidney function and individual needs.
Types of Peritoneal Dialysis:
- Continuous Ambulatory Peritoneal Dialysis (CAPD): In CAPD, the patient manually performs the dialysate exchanges several times a day, without the need for a machine. Each exchange typically takes 30-40 minutes.
- Automated Peritoneal Dialysis (APD): APD involves the use of a machine (cycler) to perform the
dialysate exchanges while the patient sleeps. This automated process
allows for greater convenience and flexibility.
Advantages: Peritoneal dialysis offers some advantages
over hemodialysis, such as more flexible treatment schedules, less dietary and
fluid restrictions, and greater control over the dialysis process. Some
patients find it more convenient and less disruptive to their daily activities.
Side Effects and Complications: Peritoneal
dialysis is generally well-tolerated, but it can be associated with potential
side effects and complications, including infection, catheter-related problems,
and issues related to the peritoneal membrane.
The choice between peritoneal dialysis and hemodialysis depends on
several factors, including the patient's health, lifestyle, and preferences.
Patients with ESRD work closely with their healthcare team to determine the
most suitable dialysis method for their specific needs. Peritoneal dialysis is
typically performed at home or in an outpatient setting and allows for a level
of independence in managing one's dialysis treatment.



.png)