- Home
- About
- Hospitals
-
Treatments
- Orthopedic & Spine
- Knee Replacement
- Carpal Tunnel Release
- Rotator Cuff Repair
- Meniscus Repair / Meniscectomy
- Total Hip Replacement (THR)
- Total Shoulder Replacement
- Arthroscopy
- Ligament Reconstruction
- Spinal Fusion
- Discectomy
- Laminectomy
- Spinal Decompression
- Vertebroplasty and Kyphoplasty
- Fracture Repair
- ACL Reconstruction
- Tendon Repair
- Osteotomy
- Amputation
- Pediatric and Adult Cardiac
- Neuroscience
- Oncology
- Nephrology & KTP
- Gastroenterology & Hepatobiliary
- Obstetrics and Gynaecology
- Infertility
- Dental & Maxillofacial
- Plastic & Cosmetic Surgery
- Rhinoplasty
- Blepharoplasty (Eyelid Surgery)
- Facelift (Rhytidectomy)
- Breast Augmentation (Mammoplasty)
- Breast Reduction (Mammoplasty)
- Breast Lift (Mastopexy)
- Liposuction
- Abdominoplasty (Tummy Tuck)
- Brazilian Butt Lift (BBL)
- Lip Augmentation
- Breast Reconstruction
- Cleft Lip and Palate Repair
- Scar Revision
- Burn Reconstruction
- Botox Injection
- Ophthalmology
- Otolaryngology (ENT)
- Endocrinology
- General and Minimal Invasive Surgery
- Pulmonology
- Rheumatology
- Urology
- General Medicine
- Multispecialty
- Orthopedic & Spine
- Doctors
- Contact Us
Heart Transplant
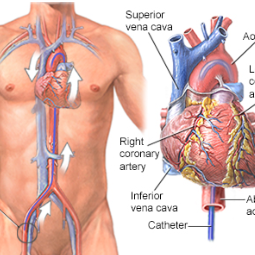
Heart Transplant is a surgical procedure in which a damaged or failing heart is replaced
with a healthy heart from a deceased donor. It is a complex and life-saving
procedure performed for individuals with end-stage heart failure or severe
heart disease when no other treatment options are effective. Heart
transplantation offers a chance for improved quality of life and extended
survival for eligible patients.
Here's an overview of heart transplantation:
Indications for Heart Transplant: Heart
transplantation is considered when a patient's heart function is severely
compromised, and they experience symptoms of advanced heart failure, such as:
- Severe heart failure: When the heart is unable to pump blood effectively to meet the body's needs, resulting in fatigue, shortness of breath, fluid retention, and other symptoms.
- Cardiomyopathy: A condition in which the heart muscle becomes weak and cannot contract adequately.
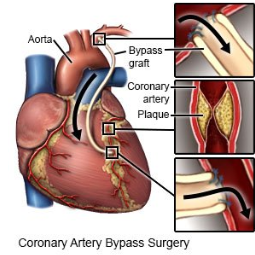
- Coronary artery disease: When multiple coronary arteries are severely blocked, leading to reduced blood supply to the heart muscle.
- Congenital heart disease:
Severe congenital heart defects that affect heart function and cannot be
corrected with other treatments.
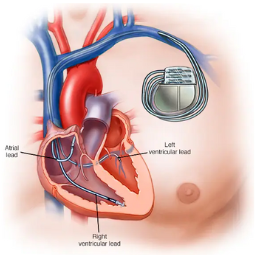
The Heart Transplant Procedure: The heart
transplant procedure involves several key steps:
- Recipient Evaluation: Before the transplant, the patient undergoes a thorough evaluation to determine their suitability for the procedure. This assessment includes medical, psychological, and social evaluations to ensure the patient can withstand the surgery and adhere to post-transplant care.
- Donor Matching: A suitable donor heart must be found, and compatibility between the donor and recipient is assessed based on factors like blood type, body size, and other medical criteria.
- Transplant Surgery: The transplant surgery is performed in an operating room under general anesthesia. The recipient's damaged heart is removed, and the donor heart is implanted in its place. The major blood vessels are carefully connected, and the new heart is positioned and secured.
- Post-Transplant Monitoring: After the surgery, the patient is closely monitored in an intensive care unit (ICU) to assess the heart's function and overall recovery.
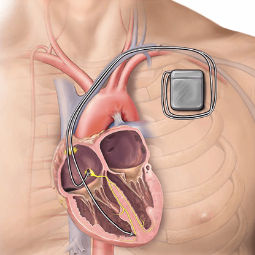
- Immunosuppression: To
prevent the recipient's immune system from rejecting the transplanted
heart, immunosuppressive medications are prescribed. These drugs need to
be taken for life to ensure the body does not attack the donor heart.
After the
Transplant: Recovery and post-transplant care are
critical for the success of the procedure:
- The patient will stay in the hospital for a period of time, typically one to two weeks or longer, to monitor the heart's function, manage any complications, and adjust medications.
- Regular follow-up visits will be scheduled for the patient to monitor heart function and manage medication regimens.
- The patient will need to make significant lifestyle adjustments and adhere to a strict medication regimen to prevent organ rejection and maintain heart health.
- Cardiac rehabilitation, which includes supervised exercise and
education on heart-healthy living, is a crucial component of the
post-transplant recovery process.
Heart transplantation can significantly improve the quality of life and
extend survival for individuals with end-stage heart failure. However, it is a
complex and major surgical procedure associated with risks and lifelong
commitments to medication and medical follow-up. The decision to pursue heart
transplantation is made based on a careful evaluation of the patient's medical
condition and individual circumstances.



.png)